
Coordinated health aid for vaccination has increased coverage rates and saved the lives of children around the world.
Foreign aid continues to have influential sceptics. A large body of research has struggled to develop a consensus, even among economists. There are two substantial challenges to studying the impact of foreign aid: (1) countries that receive aid differ in other dimensions from countries that do not, making comparisons fraught, and (2) the impact of foreign aid is multifaceted, making it difficult to identify relevant short- and long-term outcomes. As suggested by many experts, contributions to this debate should focus on rigorously evaluating programmes with a tight link between the aid and the targeted outcomes (Bourguignon and Sundberg 2007, Easterly 2003, Bates et al. 2007, Banerjee and Duflo 2011, Qian 2015).
In our research, we evaluate the impact of the more than US$16 billion in funding that Gavi, the Vaccine Alliance, has distributed to low- and middle-income countries for vaccination expansion since 1999 (Shastry and Tortorice 2025). We show that Gavi’s vaccine support increased coverage rates by a modest 2-5 percentage points on average. However, Gavi has also played a key role in making vaccines that target the pneumococcal and rotavirus diseases available in the developing world (Kremer et al. 2020). Gavi’s support for these new vaccines increased coverage by 10-20 percentage points.
We also demonstrate the value of Gavi-supported vaccination for child health. Gavi’s support for a vaccine reduced child mortality from related causes by one child per 1,000 live births. We estimate that health aid distributed through Gavi over the past 20 years has saved approximately 1.5 million lives.
Since 1999, Gavi has provided over $16 billion in funding for vaccination around the world
Gavi, the Vaccine Alliance, was created in 1999 by the Bill and Melinda Gates Foundation, the World Health Organization, UNICEF, and the World Bank. Sovereign donors soon began providing additional support, making up half of all donations to Gavi by 2005 (Chee et al. 2008). From 1999 to 2016, Gavi distributed about 40% of all foreign aid for immunisation (Ikilezi et al. 2021), including $2 billion of aid from the United States through USAID (USAID 2024).
Gavi distributes funds to low- and middle-income countries (LMICs) to purchase vaccine doses, as well as grants to strengthen health systems and improve vaccine delivery. Most of this funding supports routine immunisation for infants. Although eligibility is determined by a country’s per-capita gross national income, countries apply for Gavi funding for each vaccine and commit to Gavi’s cost-sharing agreement, contributing $0.20 per dose. Initially, Gavi focused on vaccines that were already available in lower-income countries such as diphtheria, pertussis, and tetanus (DPT), but, since 2008, Gavi has funded vaccines that were largely unavailable in these countries such as pneumococcal and rotavirus vaccines. These vaccines target lower respiratory infections and diarrheal diseases, two leading causes of death among young children.
How did Gavi support increase vaccine coverage over time?
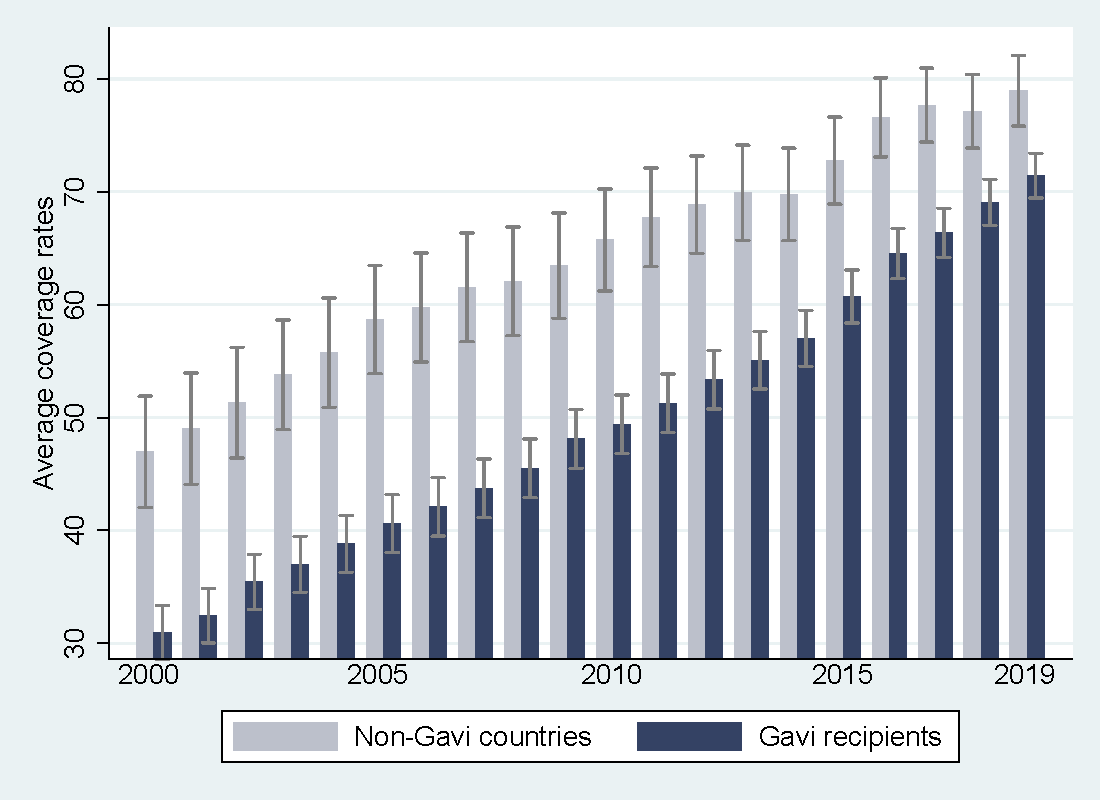
A first glance at the data suggests that Gavi support has increased vaccine coverage in recipient countries for funded vaccines; however, it also highlights the difficulty in identifying the causal effect of that support. Figure 1 illustrates vaccine coverage over time for Gavi recipients (dark blue) and non-Gavi lower-income countries (light grey) using WHO/UNICEF estimates. This demonstrates the dramatic increase in vaccine coverage since Gavi’s founding among recipients, bridging the gap between Gavi and non-Gavi countries. However, it is also clear that Gavi recipients differed significantly from non-Gavi recipients initially, making it difficult to attribute the relative increase in coverage to Gavi funding.
Would Gavi recipients have closed the gap in coverage even in the absence of Gavi support? Previous research provides conflicting responses to that question. While Jaupart et al. (2019) attribute this differential growth in coverage to Gavi, Dykstra et al. (2019) argue that Gavi recipients would have witnessed this differential growth anyway.
Figure 1: Vaccine coverage over time
In our paper, we use a new strategy to answer this question, leveraging additional variation across countries depending on when Gavi provided support for each vaccine. Instead of comparing Gavi recipients to non-Gavi recipients as in previous studies, we compare coverage for Gavi-funded vaccines to that of non-Gavi-funded vaccines within the same birth cohort and country. This allows us to control for time-varying differences across countries, vaccine-specific global trends, and country-specific differences across vaccines.
The following heuristic example illustrates our strategy. Consider two countries, Niger and Senegal. While Senegal received Gavi funding for the measles vaccine in 2013, Niger received it in 2019. Neither ever received Gavi funding for the BCG vaccine. According to survey estimates, Senegal saw a 5.6 percentage point increase in measles vaccine coverage, but only a 1.8 percentage point increase in BCG coverage, between 2011 and 2015 (World Health Organization , n.d.). Niger also saw increases in measles vaccine and BCG coverage between these birth cohorts, but by the same amount (7.4 percentage points).
We can attribute the 3.8 (5.6 minus 1.8) percentage point difference to Gavi support if we are assuming that, absent Gavi funding for the measles vaccine, Senegal would have witnessed a similar increase in measles and BCG coverage, as Niger did. Note that we do not have to assume that Senegal and Niger would have seen the same increase in measles vaccine coverage; other differences between these countries would make this suspect. Our strategy averages across many examples like this one.
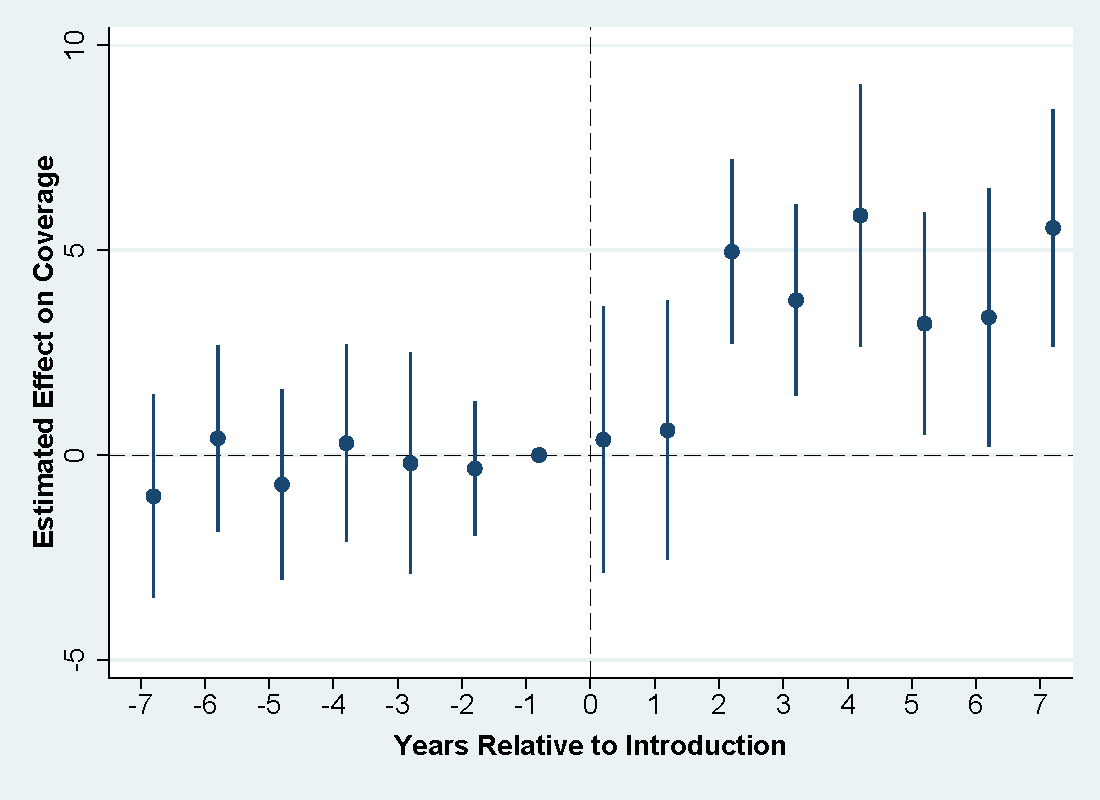
Figure 2 displays the conditional difference between the coverage of funded and unfunded vaccines relative to the year before Gavi began funding the vaccine. Importantly, there is no difference prior to Gavi funding; in other words, coverage of funded vaccines was trending similarly to other vaccines prior to funding, supporting the cross-vaccine comparisons we study. After Gavi support, we see a 3-5 percentage point increase in coverage of funded relative to unfunded vaccines.
Many of the vaccines that Gavi supports were already available in LMICs. Conducting this analysis by groups of vaccines, we document a statistically significant, but smaller 2-4.5 percentage point increase for pre-existing vaccines, such as DPT and measles, and a much larger 10-20 percentage point increase for the pneumococcal and rotavirus vaccines.
Figure 2: Impact of Gavi-funded introduction of a vaccine on coverage rate
How did Gavi support affect child health?
We also evaluate the impact of Gavi support on child mortality. As we did with vaccines, we compare child mortality across countries and time, as well as across causes of death, some of which would have been affected by funded vaccines. This comparison allows us to control for varying trends in child mortality across countries, requiring only that we assume that differences in trends across causes of death are similar across countries. For example, in countries that received Gavi support for the pneumococcal vaccine, but not the rotavirus vaccine, we would expect a greater decline in deaths from respiratory infections than from diarrheal diseases, relative to countries that did not receive Gavi support for either vaccine.
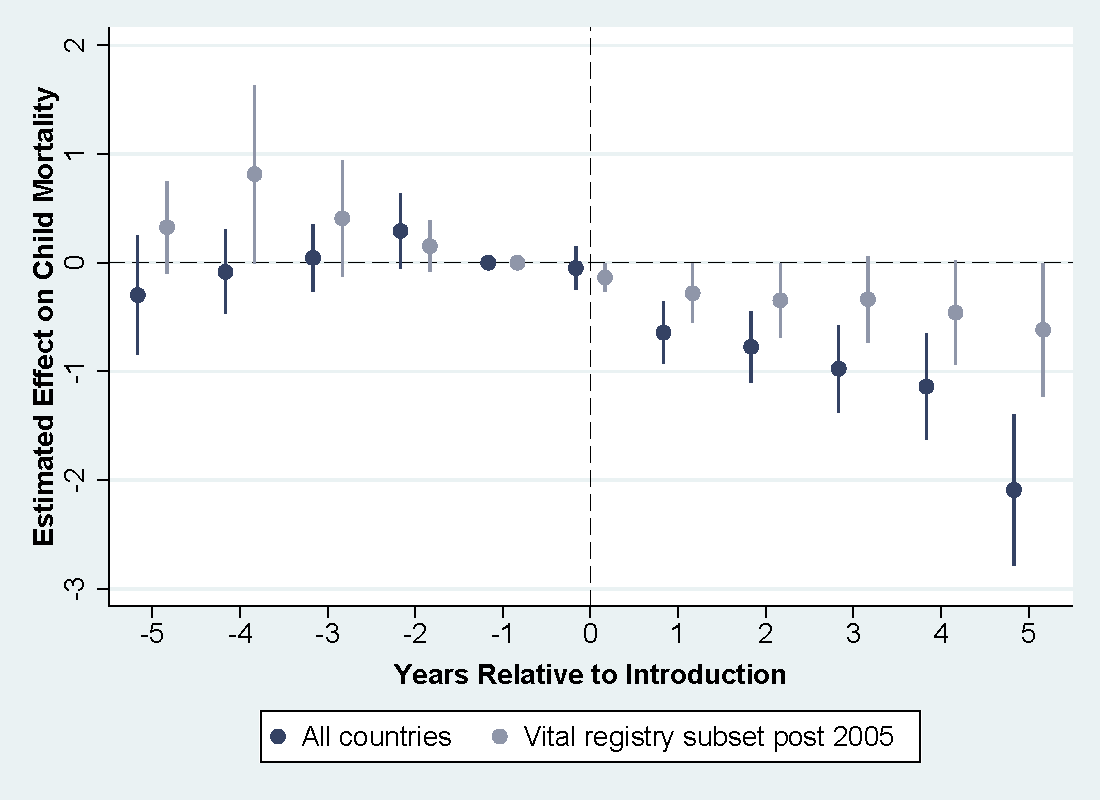
We study this using mortality data for children aged 1-59 months, measuring deaths per 1,000 live births across 15 different causes (Perin et al. 2022). Since data on mortality-by-cause in LMICs is often imputed due to data availability, we focus our analysis on the subset of countries that have vital registry data. Figure 3 displays the conditional difference in child mortality between causes of death affected by a Gavi-funded vaccine and other causes, relative to the year before the vaccine was introduced, for all countries and for the vital registry subset. We see significant reductions in child mortality from causes targeted by the supported vaccines of about one child per 1,000 live births for each vaccine introduced. These reductions are driven by declines in respiratory and diarrheal deaths, two leading causes of child mortality.
Figure 3: Impact of Gavi-funded vaccine introduction on child mortality by cause
Policy implications for health aid
We use our estimates on the impact of Gavi funding on child mortality to calculate the number of lives saved by Gavi support, which is approximately 1.5 million lives. Using cost estimates from Gavi, we estimate that each life was saved for less than $9,000. However, we view these figures as lower bounds on the impact of Gavi aid, as Gavi programmes generate additional long-term impacts on health and productivity.
Not only are these findings pivotal to shaping global health policy, but they also have important implications for the future of health aid. Providing vaccines to LMICs saves the lives of the world’s poorest children at a very low cost, making this form of aid an exceptionally cost-effective way to do good.
References
Banerjee, A V, and E Duflo (2011), Poor economics: A radical rethinking of the way to fight global poverty, PublicAffairs, New York.
Bates, R H, A Deaton, J N Bhagwati, A V Banerjee, A H Amsden, and N Stern (2007), Making aid work, MIT Press, Cambridge, MA.
Bourguignon, F, and M Sundberg (2007), “Aid effectiveness—opening the black box,” American Economic Review, 97(2): 316–321.
Chee, G, V Molldrem, N His, and S Chankova (2008), Evaluation of Gavi Phase 1 Performance, Bethesda, MD: Abt Associates Inc.
Dykstra, S, A Glassman, C Kenny, and J Sandefur (2019), “Regression discontinuity analysis of Gavi's impact on vaccination rates,” Journal of Development Economics, 140: 12–25.
Easterly, W (2003), “Can foreign aid buy growth?” Journal of Economic Perspectives, 17(3): 23–48.
Ikilezi, G, A E Micah, S D Bachmeier, I E Cogswell, E R Maddison, H N Stutzman, G Tsakalos, L Brenzel, and J L Dieleman (2021), “Estimating total spending by source of funding on routine and supplementary immunisation activities in low-income and middle-income countries, 2000–17: A financial modelling study,” The Lancet, 398(10314): 1875–1893.
Jaupart, P, L Dipple, and S Dercon (2019), “Has Gavi lived up to its promise? Quasi-experimental evidence on country immunisation rates and child mortality,” BMJ Global Health, 4(6).
Kremer, M, J Levin, and C M Snyder (2020), “Advance market commitments: Insights from theory and experience,” AEA Papers and Proceedings, 110: 269–273.
Qian, N (2015), “Making progress on foreign aid,” Annual Review of Economics, 7: 277–308.
Perin, J, A Mulick, D Yeung, F Villavicencio, G Lopez, K L Strong, D Prieto-Merino, S Cousens, R E Black, and L Liu (2022), “Data and code to reproduce estimates from ‘Progress towards the Sustainable Development Goals: A systematic analysis for estimating global, regional, and national causes of under-five mortality during 2000–2019’,” https://github.com/amulick/MCEE-u5mort2019, accessed 14 March 2022.
Shastry, G K, and D Tortorice (2025), “Effective health aid: Evidence from Gavi’s vaccine program,” Applied Economic Journal: Economic Policy, 17(1): 540–574.
USAID (2024), “USAID’s investment to Gavi, the Vaccine Alliance,” https://2017-2020.usaid.gov/sites/default/files/documents/1864/GAVI_factsheet_4_16-508.pdf, accessed 10 February 2025.
World Health Organization (n.d.), “Immunization, vaccines and biologicals, coverage survey data [Data Table],” https://immunizationdata.who.int/global?topic=&location=, accessed 31 October 2019.


