
Lowering peak pollution exposure through fuel efficient cookstoves reduces respiratory symptoms. But in areas with high average pollution, more must be done to improve clinical outcomes and reduce health expenditures.
Air pollution is “the single biggest environmental threat to human health” (WHO 2021). The Global Burden of Disease study (Lancet 2017) estimates that it is responsible for 7–9 million premature deaths annually (10-15% of all deaths), and 90% of pollution related deaths occur in low- and middle-income countries (WHO 2021).
Existing evidence indicates that high average levels of pollution exposure negatively impact health (Deryugina and Reif 2023, Schlenker and Walker 2015, Greenstone and Hanna 2014). However, many economic activities—such as commuting and cooking—cause large, brief spikes in exposure which only modestly impact one’s daily average levels. In low- and middle-income countries where more than four billion people do not have access to clean cooking technologies (World Bank 2020), traditional biomass cookstoves can cause significant spikes in pollution exposure. 66% of Kenyan households use a biomass fuel for cooking and 42% use a traditional ceramic cookstove fueled by charcoal (known colloquially as a “jiko”). According to the World Bank’s Kenya Country Environmental Analysis (2019), “those who cook inside with poor ventilation have 400–600 µg/m3 average annual concentration of PM2.5 in their household.” These levels are extremely high, even compared with the WHO’s least stringent air pollution target of <35 µg/m3 (WHO 2021).
Figure 1: Daily pollution for two study participants, both with average exposure of 21 µg/m3
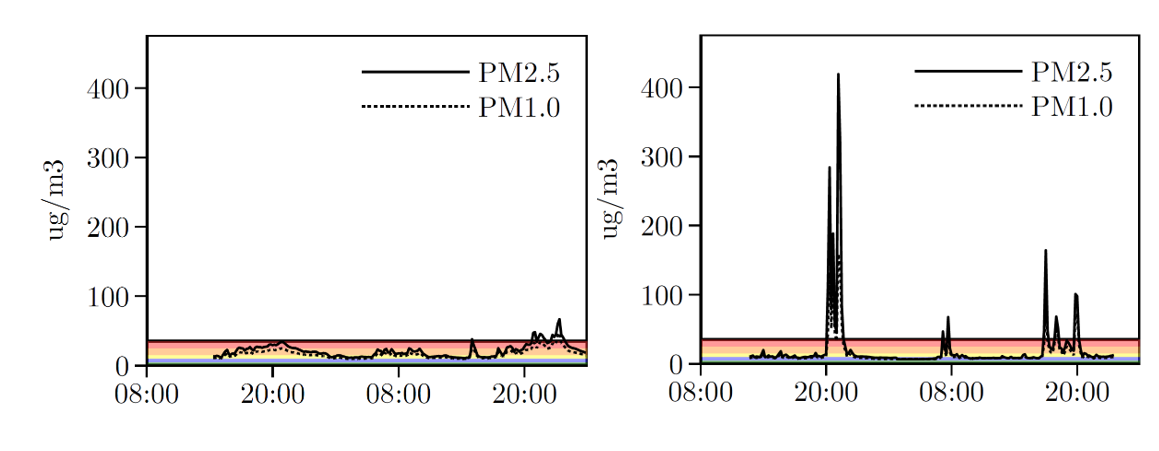
Notes: Two individuals who have identical average exposure, but significantly different within day exposure to peaks. The colored bars represent different WHO pollution regulations, which correspond to 0-5, 5-10, 10-15, 15-25, and 25-35 µg/m3.
In a randomised field study involving 700 low-income families in Nairobi, Kenya, we use the Becker-DeGroot-Marschak (1964) mechanism to induce random variation in adoption of an improved charcoal cookstove (known as a “Jikokoa”). We study how fuel-efficient cookstove adoption impacts pollution exposure and health after three years of stove ownership (Berkouwer and Dean 2023). How effective are improved, fuel efficient cookstoves at reducing spikes in pollution exposure? And how does a persistent reduction in the repeated exposure to spikes caused by these activities impact health?
Answering these questions will inform how we think about regulatory policies to efficiently minimise the adverse effects of pollution on health. Most countries–and the WHO–provide standards for the daily and annual average concentrations of particulate matter (PM2.5) and carbon monoxide (CO), but these standards “mask sharp PM2.5 concentration spikes over short periods of minutes to hours” (Nazarenko et al. 2021). In part due to the lack of evidence, standards for sub-daily peaks are subject to ongoing regulatory debate (EPA 2023).
Improved cookstoves decrease spikes by 42%, but have no significant influence on average pollution levels
Studying the impact of short-term pollution spikes requires high-frequency data on pollution exposure and time-use (what activities are being done at any given hour) for each individual. To collect this data, study participants carry a backpack containing a Purple Air (PA-II) device and a Lascar device for 48-hours. The PA-II device measures PM2.5 concentrations every two minutes, and the Lascar device measures CO levels every minute. Then, study participants recount their activities, such as cooking or traveling on a bus, for each hour where they carried the devices. This allows us to identify which activity a participant was doing when they experienced a spike in pollution.
From this data, we find that improved cookstoves reduce peak cooking emissions by 42%, or about 52 ug/m3. Since the improved cookstove also reduces total cooking time, the total reduction in pollution exposure while cooking is 48%.
Figure 2: Impact of adoption on pm 2.5 exposure
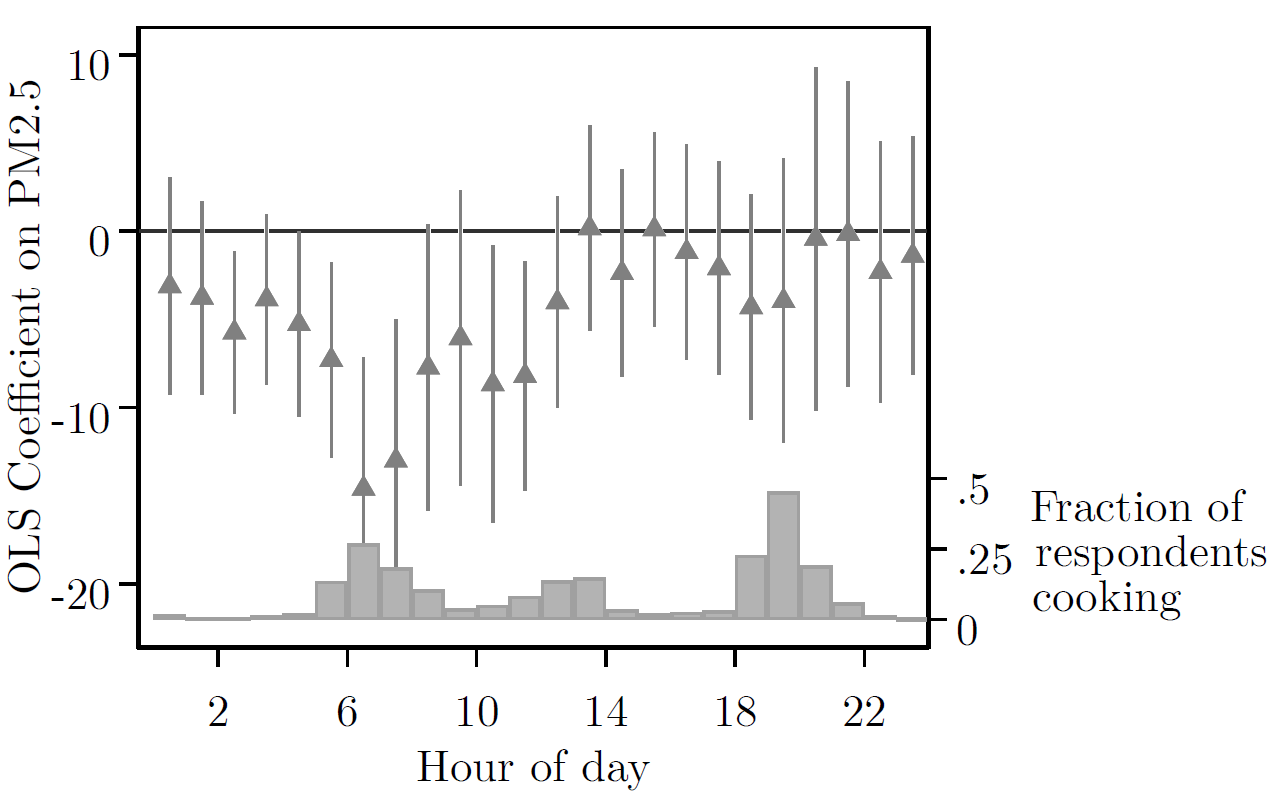
Notes: Pollution exposure for adopters decreases significantly relative to non-adopters when many participants are cooking, but is otherwise unchanged.
However, despite this large difference in peaks, the improved cookstove caused only a 2% reduction on average pollution over the 48-hours where the device was worn, and this is not statistically different from zero. This is because participants cook on average only two hours a day: for the remaining 22 hours per day, study participants are exposed to Nairobi’s high levels of ambient pollution (~25 ug/m3).
Reduced spikes reduce respiratory symptoms, but have limited effect on some major clinical outcomes
How does the 42% reduction in peaks impact health? To answer this question, we follow the methodology from field experiments in the public health literature (see for example Tielsch et al. 2016, Smith-Sivertsen et al. 2009, Checkley et al. 2021 and others). We measure study participants’ blood pressure and blood oxygen levels using a sphygmomanometer and pulse oximeter (following the methodology set by the CDC 2019). We ask study participants whether a medical professional has diagnosed them with certain conditions or diseases (such as pneumonia) and whether they’ve experienced specific respiratory and non-respiratory symptoms in recent weeks. Respiratory symptoms include sore throat, headache, cough, and runny nose while non-respiratory symptoms include stomach pain, skin rash, or muscle pain (myalgia). We also ask how much they have spent on health-related expenditures in recent months.
We estimate that adoption of fuel efficient cookstoves causes people to be significantly less likely to report experiencing respiratory related symptoms. This is an important health benefit: reducing the magnitude and duration of spikes in exposure can reduce short-term unpleasant symptoms.
However, we do not find that cookstove adoption leads to improvements in other major, long-term clinical outcomes. We find no significant difference in blood pressure or blood oxygen levels, likelihood to be diagnosed with any disease or condition (including pneumonia), or health care related expenditures. The lack of reduction in aggregate average pollution exposure may explain the lack of impacts on chronic or quantitative health outcomes. While reductions in peak exposure can generate important short-term reduction in symptoms, improvements in long-term measures of health may require reductions in ambient air pollution exposure.
Fuel-efficient cookstove adoption improves well-being and peak pollution exposure, but has limited effects on health
While the literature has shown that cookstove adoption can improve financial well-being (Bensch et. al. 2015, Berkouwer and Dean 2022 and others), there is limited evidence on the causal effect of adoption on pollution and health. This is especially true in urban settings. We show that adoption significantly reduces peak pollution exposure, but given that adopters continue to experience high levels of ambient pollution for the remaining 22 hours per day, this leads to insignificant changes to average pollution. This reduction in peaks causes improvements in short-term respiratory health, but does not meaningfully impact major clinical outcomes.
Our results suggest that individuals have only limited ability to improve their health via fuel-efficient technology adoption when they experience high levels of ambient pollution daily. Reducing pollution-related health complications in urban settings may require stricter regulation of ambient pollution. These results also suggest that accounting for shorter-period averages in emissions regulations can improve health, but not as much as stricter regulation on daily or yearly average pollution levels.
References
Becker, G M, M H Degroot, and J Marschak (1964), "Measuring utility by a single-response sequential method", Systems Research and Behavioral Science, 9(3): 226–232.
Bensch, G, M Grimm, and J Peters (2015), "Why do households forego high returns from technology adoption? Evidence from improved cooking stoves in Burkina Faso", Journal of Economic Behavior & Organization, 116: 187–205.
Berkouwer, S B and J T Dean (2022), "Credit, attention, and externalities in the adoption of energy efficient technologies by low-income households", American Economic Review, 112(10).
Berkouwer, S B and J T Dean (2023), “Private Actions in the Presence of Externalities: The Health Impacts of Reducing Air Pollution Peaks but not Ambient Exposure” NBER Working Paper no w31614.
Centers for Disease Control and Prevention (2019), "National Health and Nutrition Examination Survey: Blood Pressure Procedures Manual".
Checkley, W, K N Williams, J L Kephart, M Fandiño-Del-Rio, N K Steenland, et al. (2021), "Effects of a Household Air Pollution Intervention with Liquefied Petroleum Gas on Cardiopulmonary Outcomes in Peru. A Randomized Controlled Trial", American Journal of Respiratory and Critical Care Medicine, 203(11): 1386–1397.
Cohen, A J, M Brauer, R Burnett, H R Anderson, J Frostad, et al. (2017), "Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015".
Deryugina, T and J Reif (2023), "The Long-run Effect of Air Pollution on Survival", Working Paper 31858, National Bureau of Economic Research.
Environmental Protection Agency (2023), "Reconsideration of the National Ambient Air Quality Standards for Particulate Matter", https://www.federalregister.gov/d/2023-00269, Docket numbers EPA-HQ-OAR-2015-0072, FRL-8635-01-OAR.
Greenstone, M and R Hanna (2014), "Environmental Regulations, Air and Water Pollution, and Infant Mortality in India", American Economic Review, 104(10): 3038–72.
Nazarenko, Y, D Pal, and P A Ariya (2021), "Air quality standards for the concentration of particulate matter 2.5, global descriptive analysis", Bulletin of the World Health Organization, 99(2): 125–137D.
Schlenker, W and W R Walker (2015), "Airports, Air Pollution, and Contemporaneous Health", The Review of Economic Studies, 83(2): 768–809.
Smith-Sivertsen, T, E Díaz, D Pope, R T Lie, A Díaz, et al. (2009), "Effect of Reducing Indoor Air Pollution on Women’s Respiratory Symptoms and Lung Function: The RESPIRE Randomized Trial, Guatemala", American Journal of Epidemiology, 170(2).
Tielsch, J M, J Katz, S K Khatry, L Shrestha, P Breysse, et al. (2016), "Effect of an improved biomass stove on acute lower respiratory infections in young children in rural Nepal: a cluster-randomised, step-wedge trial", The Lancet Global Health, 4, S19.
World Bank Group (2019), "Kenya Country Environmental Analysis".
World Bank Group (2020), "The State of Access to Modern Energy Cooking Services".
WHO (2021), "WHO global air quality guidelines: Particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide".

