
Ageing pipe systems and the absence of complementary sanitation investments compromise the health benefits of water disinfection
Large-scale investments in municipal water quality played a critical role in improving health outcomes in high-income countries. The implementation of disinfection technologies such as chlorination in the late 19th and early 20th centuries led to the near elimination of mortality from diarrhoeal diseases in the United States and Japan (Cutler 2018, Ferrie and Troesken 2008, Inoue and Ogasawara 2020). Over time, lower- and middle-income countries also adopted the same disinfection technologies. However, in contrast to the experience of higher-income countries, diarrhoeal diseases remain prevalent in many lower-income countries.
Why has this been the case? Understanding the reasons for lower returns to water disinfection in lower-income countries is critical given that diarrhoeal diseases are still the third leading cause of child mortality worldwide (Roser et al. 2013, GBD 2016 Diarrhoeal Disease Collaborators 2018). Moreover, the projected rapid growth of cities over the next three decades will require massive new investments in water infrastructure in many urban areas (United Nations 2019). Ensuring maximal return on such costly investments is a key goal for policymakers.
Understanding the limited health benefits from water disinfection in lower-income countries
Scientific literature suggests two possible explanations. First, disinfection programmes in lower-income countries were introduced into much older municipal pipe water systems. As water pipe systems age, pipe breaks and interruptions in water flow become more common, introducing disease-causing pathogens and infecting the water (Ercumen et al. 2015, Kumpel and Nelson 2014, Lee and Schwab 2005). Consistent with this, cross-country data reveal that diarrhoeal disease mortality rates increase with the higher frequency of pipe breaks, a correlation that persists after adjusting for GDP per capita (Figure 1).
Figure 1 Pipe break frequency is correlated with diarrhoeal disease death rate
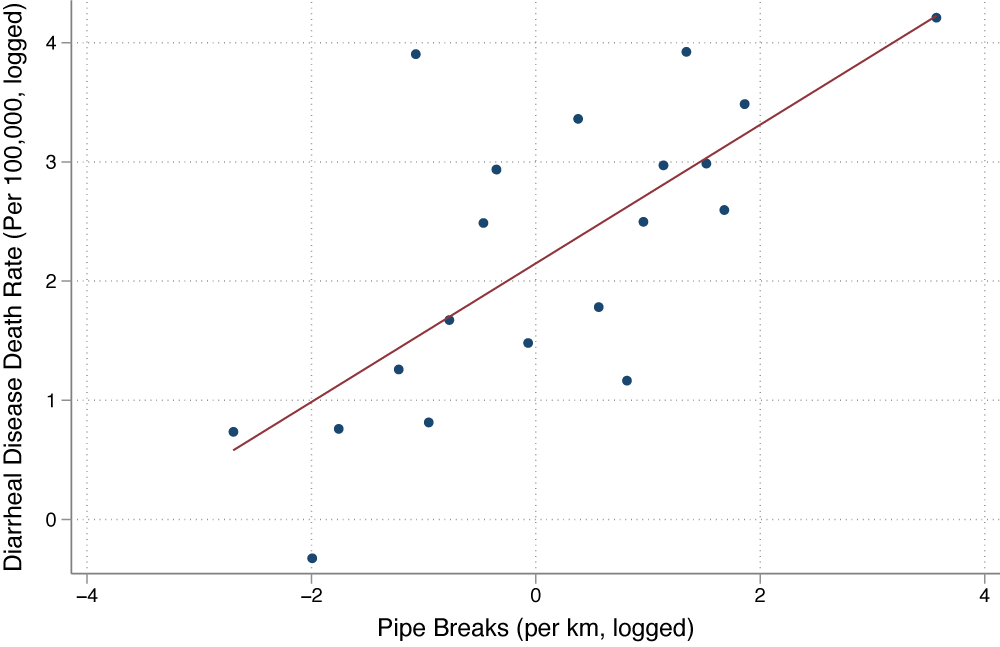
Note: Piped-water infrastructure quality and diarrhoeal disease mortality rates for a sample of 42 low- and middle-income countries with available data on all measures. Countries are grouped into 20 equal-sized ventiles of infrastructure quality measure.
Second, the health benefits of water disinfection are larger when complementary infrastructure investments in sanitation —a key driver of waterborne disease risk— are made (Alsan and Goldin 2019, Duflo et al. 2015). However, resource constraints have precluded many lower-income countries from making these complementary investments on a large-scale (World Bank 2017).
There are few systematic assessments of muted returns to water disinfection in lower-income countries. In a new study, we attempted to fill this evidence gap by using a large-scale water programme adopted in Mexico (Bhalotra, Diaz-Cayeros, Miller, Miranda, and Venkataramani 2021).
Mexico’s Programa Agua Limpia
Programa Agua Limpia (PAL) was introduced in 1991 as a means to mitigate the potential public health consequences of a cholera epidemic, which was then spreading through neighbouring countries (Sepúlveda et al. 2006). The focus of this US$1.9 billion1 programme was the chlorination of drinking water in small and medium-sized cities (the larger cities already had chlorination coverage).
The programme was national in scope and was swiftly executed. Between April and December 1991, the share of urban residents with access to chlorinated water increased sharply from 58% to over 90%. The rollout was quick because existing piped water systems were used to deliver the disinfected water. In addition, Mexican municipalities varied in pre-programme sanitation infrastructure. Thus, the PAL is a natural experiment implemented in a setting well suited to examining the laid-out hypotheses.
Impacts of water chlorination on diarrhoeal disease mortality
We assessed the impacts of the PAL on diarrhoeal disease mortality among children under five years of age given their high vulnerability at this age. A challenge to estimating causal effects of the PAL is that data on the exact placement and timing of chlorination infrastructure were not available. However, in addition to the speed of national implementation, two other features of the PAL allow us to identify causal effects. First, investments in water quality predominantly affect infectious diarrhoeal diseases. Second, the programme targeted cities of a specific size. These features allowed us to employ a series of complementary difference-in-differences strategies.
Specifically, we compared diarrhoeal disease mortality rates, before and after the PAL, in small and medium-sized cities relative to changes in mortality from diseases less affected by water quality. We considered respiratory infections and non-infectious diseases (such as perinatal conditions and congenital malformations). Respiratory infections share many of the same risk factors as diarrhoeal diseases, with the notable exception of water quality (Ahuja et al. 2010). However, as individuals affected by diarrhoea are more susceptible to contracting other infections (Walker et al. 2013, Inoue and Ogasawara 2020), we used non-infectious disease mortality as an alternative control. In a second difference-in-differences design, we compared changes in diarrhoeal disease mortality between small- and medium-sized cities against changes in larger cities.
These different approaches yielded similar conclusions. Using individual-level death certificate data (aggregated to municipality-level) for 1985-1995, we estimated that the PAL led to a 45-67% reduction in diarrhoeal disease mortality (Figure 2). These estimates – equivalent to approximately 9,100–16,000 deaths averted between 1991 and 1995 – imply a cost per life year saved of US$1,900–3,400. These estimates are conservative as they do not account for programme impacts accruing after 1995, or the long-run health and labour market effects of reduced exposure to childhood diarrhoea among surviving children (Bhalotra et al. 2021). Even so, we conclude the PAL was highly cost-effective.
Figure 2 Under-five mortality rates before and after the PAL
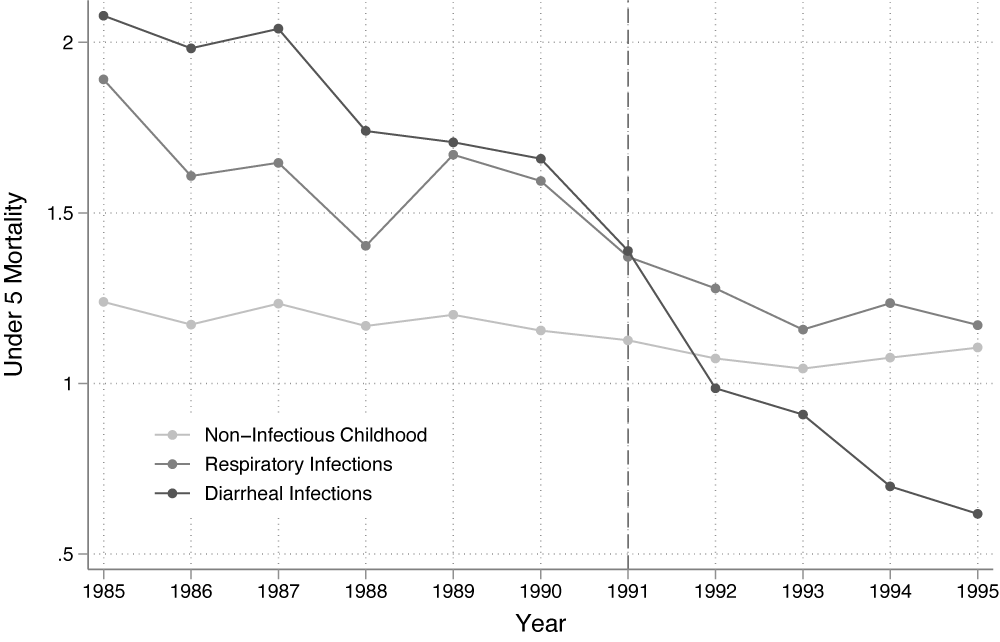
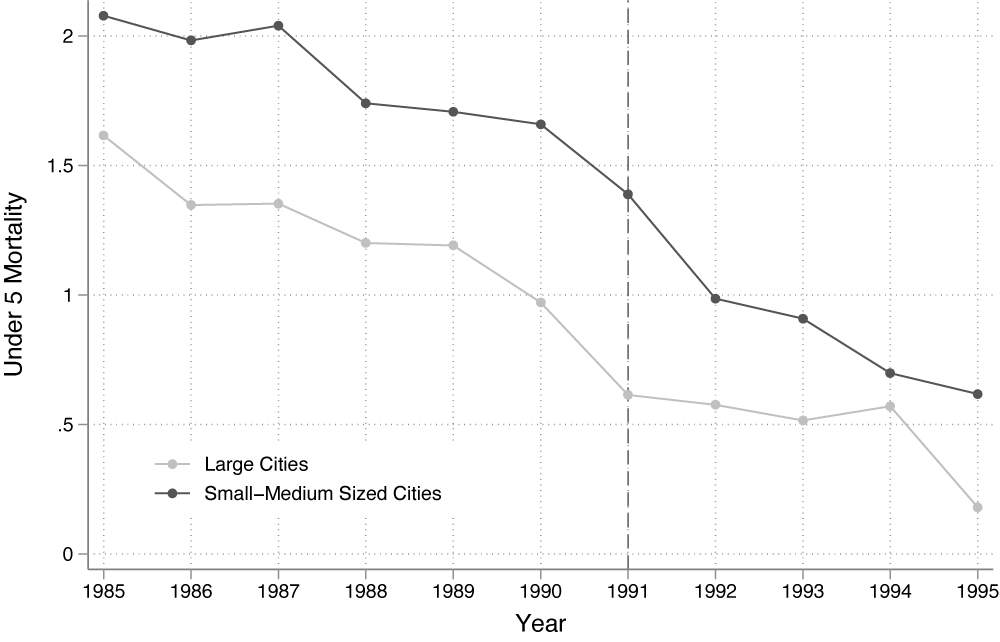
Note: Trends in under-five mortality rates, 1985-1995. Panel A plots trends in diarrhoeal disease mortality rates against mortality from respiratory infections and non-infectious causes (control disease). Panel B plots trends in diarrhoeal disease mortality rates between small and medium-sized cities, which were targeted by the PAL, versus larger cities, which were not. In both panels, the dashed vertical line denotes the year the PAL was implemented.
The role of infrastructure quality and complementary investments
The estimated decline in diarrhoeal disease mortality varied greatly across cities. Our analysis showed that both dilapidated piped water infrastructure and the lack of complementary investments in sanitation attenuated the programme impact. The first clue that the integrity of water pipe infrastructure played a role in diarrhoeal disease mortality is seen in the PAL programme outcomes. These were no larger in municipalities where a greater proportion of residents had access to piped water than in others, even though PAL used existing pipe infrastructure to deliver disinfected water. We show that this is because municipalities with greater piped water coverage tended to have older systems more prone to pipe breaks. In contrast, the PAL’s impact was larger in areas with greater sewage system coverage, consistent with the complementarity noted in American history (Alsan and Goldin 2019) and in other lower-income countries (Duflo et al. 2015).
Under ideal infrastructure conditions, we estimated that the PAL would have reduced childhood diarrhoeal disease mortality by nearly 90% by 1995, a figure consistent with the historical experience of higher income countries. Accounting for the costs of upgrading and extending piped water and sewage infrastructure, we estimate a cost per life year saved of US$4,400. Thus, even without accounting for the longer time horizon over which health benefits may be realised or potential non-health benefits (Ashraf et al. 2021), this suggests that such large-scale investments in water and sanitation infrastructure are cost-effective.
Policy implications
Our results demonstrate that achieving substantial improvements in drinking water quality in lower-income countries will require upgrading existing piped water networks and ensuring complementary investments in sanitation. They show that these investments can improve population health in a cost-effective manner. However, the upfront costs of these initiatives may be prohibitive for many lower-income countries. Given that many countries are falling short in meeting financing targets (World Bank 2017), innovative approaches to financing will be needed to ensure broader access to clean water (McGuckin 2021, Cutler and Miller 2007).
References
Ahuja, A, M Kremer, and A P Zwane (2010), “Providing Safe Water: Evidence from Randomized Evaluations”, Annual Review of Resource Economics 2(1): 237–56.
Alsan, M, and C Goldin (2019), “Watersheds in Child Mortality: The Role of Effective Water and Sewerage Infrastructure, 1880–1920”, Journal of Political Economy 127(2): 586–638.
Ashraf, Na, E Glaeser, A Holland, and B M Steinberg (2021), “Water, Health and Wealth: The Impact of Piped Water Outages on Disease Prevalence and Financial Transactions in Zambia”, Economica 88(351): 755–81.
Bhalotra, S R (2020), “Clean Water Programmes Can Improve Cognitive Development”, Advantage Magazine, Pollution and Climate Change Special, 20 October.
Bhalotra, S R, A Diaz-Cayeros, G Miller, A Miranda, and A S Venkataramani (2021), “Urban Water Disinfection and Mortality Decline in Lower-Income Countries”, American Economic Journal: Economic Policy 13(4): 490–520.
Cutler, D M, and G Miller (2005), “The Role of Public Health Improvements in Health Advances: The Twentieth-Century United States”, Demography 42 (1):1-22.
Cutler, D M, and G Miller (2007), “Water, Water Everywhere: Municipal Finance and Water Supply in American Cities”, in Corruption and Reform, Chicago: University of Chicago Press.
Duflo, E, M Greenstone, R Guiteras, and T Clasen (2015), “Toilets Can Work: Short and Medium Run Health Impacts of Addressing Complementarities and Externalities in Water and Sanitation”, NBER Working Paper 21521.
Ercumen, A, B F Arnold, E Kumpel, Z Burt, I Ray, K Nelson, and J M Colford Jr (2015), “Upgrading a Piped Water Supply from Intermittent to Continuous Delivery and Association with Waterborne Illness: A Matched Cohort Study in Urban India”, PLoS Medicine 12(10): e1001892.
Ferrie, J P, and W Troesken (2008), “Water and Chicago’s Mortality Transition, 1850–1925”, Explorations in Economic History 45(1): 1–16.
Troeger, C, B F Blacker, I A Khalil, P C Rao, S Cao, S R Zimsen, S B Albertson, J D Stanaway, A Deshpande, Z Abebe, and N Alvis-Guzman (2018), “Estimates of the Global, Regional, and National Morbidity, Mortality, and Aetiologies of Diarrhoea in 195 Countries: A Systematic Analysis for the Global Burden of Disease Study 2016”, The Lancet. Infectious Diseases 18(11): 1211–28.
Inoue, T and K Ogasawara (2020), “Chain Effects of Clean Water: The Mills–Reincke Phenomenon in Early 20th-Century Japan”, Economics & Human Biology 36(January): 100822.
Kumpel, E, and K L Nelson (2014), “Mechanisms Affecting Water Quality in an Intermittent Piped Water Supply”, Environmental Science & Technology 48(5): 2766–75.
Lee, E J and K J Schwab (2005), “Deficiencies in Drinking Water Distribution Systems in Developing Countries”, Journal of Water and Health 3(2): 109–27.
McGuckin, R (2021), “Delivering Investable Water Solutions in Developing Countries”, WaterWorld, 4 October.
Roser, M, H Ritchie, and B Dadonaite (2013), “Child and Infant Mortality”, Our World in Data.
Sepúlveda, J, J L Valdespino, and L García-García (2006), “Cholera in Mexico: The Paradoxical Benefits of the Last Pandemic”, International Journal of Infectious Diseases 10(1): 4–13.
United Nations (2019), World Urbanization Prospects: The 2018 Revision, New York: United Nations Population Division.
Walker, C L F, J Perin, J Katz, J M Tielsch, and R E Black (2013), “Diarrhea as a Risk Factor for Acute Lower Respiratory Tract Infections among Young Children in Low Income Settings”, Journal of Global Health 3(1): 010402.
World Bank (2017), The World Bank Annual Report 2017
Endnotes
[1] All US$ figures are in 2015 US dollars.





