
Physical proximity to pathogen-free water sources reduces child and adult mortality
Diarrhoea is the fifth most common cause of death among children under five in the world. It is the eighth most common cause of death among adults over 70. While the public health literature recognizes unsafe water as a key risk factor for diarrhoea (Troeger et al. 2018), the relationship between water infrastructure and mortality remains widely disputed (Cutler and Miller 2005, Jamison 2018, Anderson et al. 2021, Kremer et al. 2022). The absence of a clear causal link has significant policy implications: clean water access is excluded from lists of recommended interventions to reduce childhood mortality - let alone adult mortality - by the WHO and other prominent centres of public health policy (Stenberg et al. 2021).
In our study (Buchmann et al. 2022), we exploit a natural experiment in Bangladesh to causally identify the impact of water infrastructure on mortality. Our study uses the surprise discovery of arsenic in groundwater which prompted a government-initiated campaign in 1999 to test millions of tubewells, or wells that pump water from underground sources, nationwide and encourage households to abandon wells that tested above 50ppb for arsenic (Ahmed et al. 2006). This campaign resulted in one of the most dramatic changes in health behaviour in recent history: for example, in Barisal, where our study takes place, the fraction of households drinking from contaminated tubewells dropped from 69% in 1999 to 1% in 2006 (Bangladesh Bureau of Statistics and Unicef 2006, Kinniburgh and Smedley 2001).
Our study
While the campaign was conducted nationwide, which households were encouraged to change their water sources was effectively random at the local level. Specifically, the geography of Bangladesh generates unusual variation in arsenic contamination: nearly all contaminated villages in Bangladesh contain pockets of arsenic-free groundwater along- side contaminated water, and these pockets are impossible to predict above ground. This makes the likelihood that a household was drawing from an arsenic-contaminated well prior to the campaign effectively exogenous at the village level (Smedley and Kinniburgh 2001).
We exploit this local variation in the presence of arsenic, paired with the timing of the nationwide testing campaign (and therefore revelation of arsenic contamination), to examine the behavioural consequence of this discovery: the shift from backyard shallow tubewells to alternative, less convenient water infrastructure. Shallow tubewells are vulnerable to arsenic contamination from groundwater, but they are also considered “the most appropriate technology in terms of microbiologically clean water” (Lokuge et al. 2004) in settings such as Bangladesh. Not only is water from shallow tubewells unlikely to be contaminated with faecal bacteria at source, but it also faces little risk of becoming contaminated at point of use: shallow tubewells are typically built within household com- pounds, minimizing storage time. In fact, such wells were constructed across Bangladesh in the 1970s and 1980s with the very purpose of reducing water-borne diseases such as cholera and dysentery, common to surface water or more distant alternative water sources (Pruss et al. 2002).
We collect novel data on the location and arsenic content of the closest shallow tubewells of approximately 3,000 households randomly sampled from 162 villages in the Barisal district of Bangladesh. Our data allow us to compare households whose shallow tubewells tested positive for arsenic contamination (and who were therefore actively encouraged to abandon these convenient water sources) to their neighbours in the same village whose wells tested negative and were deemed safe for drinking. We combine this spatial variation with annual data on child and elderly mortality from before and after the public health campaign to estimate the impact of switching away from backyard shallow tubewells on mortality.
The impact of abandoning contaminated tubewells
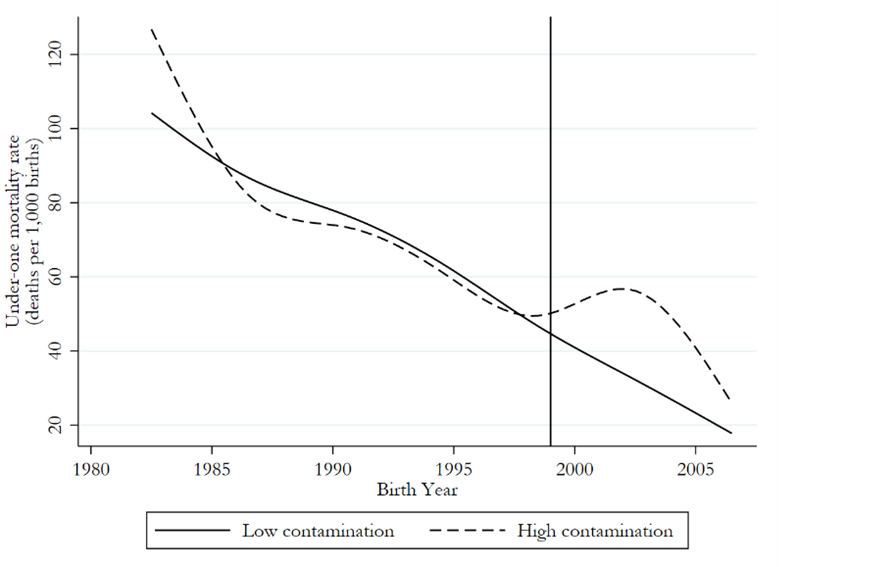
Figure 1 displays our first main result. We find that child mortality rates were almost identical in households with arsenic-contaminated versus uncontaminated shallow tubewells within villages before the arsenic campaign. But mortality diverged sharply thereafter, with households who were encouraged to switch water sources experiencing a 28% increase in child mortality relative to those with arsenic-free wells. Using cause of death data, we find that this divergence is driven by water-borne pathogen-related deaths only, with no change in arsenic-related deaths.
Figure 1: Under 1 mortality rate (0 - 1 years), four-year unadjusted averages
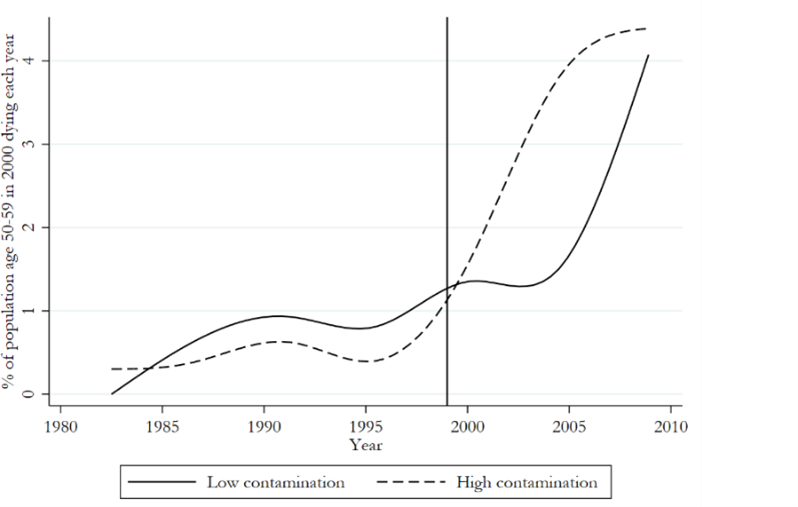
While children are vulnerable to diarrhoeal disease but less susceptible to arsenic-induced cancers (Vahter 2008, Liaw et al. 2008, Tofail et al. 2009), the elderly potentially face competing mortality risks from the two, making the impact of switching away from arsenic-contaminated but convenient shallow tubewells ex ante ambiguous in this population. However, as demonstrated in Figure 2, elderly mortality prior to the campaign appears to be similar across households drawing from arsenic-contaminated and uncontaminated shallow tubewells. After the campaign, counter to its own aims, we document that the hazard of dying for adults over 50 years old increases by 47% among households encouraged to abandon their wells, driven again by diarrhoea-related rather than arsenic-related deaths.
Figure 2: Death rate among adults age 50 - 59 in 2000, unadjusted averages
Proximity of water infrastructure is essential
Finally, we show that the rise in mortality is a consequence of inconvenience, or distance to safe water infrastructure, rather than the quality of the water itself. In Barisal, most households had access to alternative arsenic- and pathogen-free water infrastructure in the form of deep tubewells at the time of the campaign. But because deep tubewells are expensive to build (at 8.5 times the cost of shallow tubewells), they are rarely constructed by households within a family compound. For the typical household, the use of a deep tubewell requires traveling a meaningful distance, and therefore collecting and storing water in containers in the home, introducing the risk that drinking water becomes contaminated at the point of use.
By exploiting variation in the proximity of deep tubewells among households who were and were not encouraged to switch water sources in our setting, we document that mortality effects increase with distance: while those who can access a clean well within 300m of their home experience no adverse mortality impacts from abandoning their backyard shallow tubewells, each additional 100m to a clean alternative source raises both child and elderly mortality. This evidence highlights how essential proximity, or convenience, is to the health of vulnerable households, despite widespread access to pathogen-free water infrastructure.
Implications for water policy
We build on a large economics literature that aims to disentangle the role of water infrastructure, public health reforms, and rising incomes in explaining the sharp declines in mortality in high- and middle-income countries (Anderson et al. 2021, Cutler and Miller 2005, Galiani et al. 2005, Devoto et al. 2012), with widely varying results for the degree to which water infrastructure alone reduces mortality. This mixed evidence is echoed in the policy-influential Disease Control Priorities 3 (Jamison 2018), which concludes that there exists limited robust evidence on the impact of clean water on mortality. Water treatment is therefore not included in lists of recommended interventions to reduce childhood mortality by DCP-3 nor the WHO (Stenberg et al. 2021). Our study provides new evidence that accessibility to pathogen-free water should meaningfully reduce not only infant and child but also elderly mortality in contexts like that of Bangladesh. Importantly, we find these mortality impacts despite being in a context where individuals frequently ingest pathogens through food and hands (Kwong et al. 2020), and access to diarrhoea treatment is affordable and widespread.
Our results further underscore the necessity of convenience in water infrastructure. While there is consensus that on-premises water supply reduces diarrhoea rates (Wolf et al. 2022), existing studies have often suffered from a number of shortcomings. These include the fact that studies typically: compare unimproved off-premises water sources to improved on-premises sources (conflating quality and convenience); lack exogeneity in infrastructure access (with the exception of Kremer et al. (2011) and Devoto et al. (2012)); and are not powered to identify impacts on mortality. By addressing some of these weaknesses, we find large impacts of proximity on both child and adult mortality. These results have direct relevance to institutions seeking to invest in water infrastructure, as determining the density of such infrastructure requires a careful assessment of the trade-off between the material costs of more construction and the health benefits of greater proximity.
Implications for arsenic policy
Our findings raise questions about how to shape public health efforts around arsenic and the use of contaminated shallow tubewells in contexts such as Bangladesh. While we find little evidence of large mortality impacts of arsenic poisoning, other recent work has found cognitive impairment from arsenic contamination (Pitt et al. 2021). Policy recommendations must therefore weigh the health effects of reducing distance to pathogen-free water against the health consequences of arsenic exposure. Our findings raise the case for permitting shallow tubewells as a legitimate drinking water source – at least for vulnerable populations – unless safe alternative sources, such as deep tubewells, are made easily accessible (Larsen 2016).
References
Ahmed, M F, S Ahuja, M Alauddin, S J Hug, J R Lloyd, A Pfaff, T Pichler, C Saltikov, M Stute and Al van Geen (2006), “Ensuring safe drinking water in Bangladesh”, Science 314: 1687-16882006.
Anderson, D M, K K Charles, D I Rees and Tianyi Wang (2021), “Water purification efforts and the black-white infant mortality gap, 1906–1938”, Journal of Urban Economics 122: 103329.
Bangladesh Bureau of Statistics and Unicef (2006), “Multiple Indicator Cluster Suvery 2006”, p. 57.
Buchmann, N, E M Field, R Glennerster and R N Hussam (2022) “The lifesaving benefits of convenient infrastructure: Quantifying the mortality impact of abandoning shallow tubewells contaminated by arsenic in Bangladesh.” Working Paper.
Cutler, D and G Miller (2005), “The role of public health improvements in health advances: the twentieth-century United States”, Demography, 42: 1–22.
Devoto, F, E Duflo, P Dupas, W Parienté and V Pons (2012), “Happiness on tap: Piped water adoption in urban Morocco”, American Economic Journal: Economic Policy 4: 68–99.
Galiani, S, P Gertler and E Schargrodsky (2005), “Water for life: The impact of the privatization of water services on child mortality”, Journal of political economy 113: 83–120.
Jamison, D T (2018), “Disease control priorities: improving health and reducing poverty”, The Lancet, 391 (10125): e11–e14.
Kinniburgh, P L and D G Smedley (2001), “Executive summary of the final report of Phase II, groundwater studies of arsenic contamination in Bangladesh”, Technical Report 2001.
Kremer, M, J Leino, E Miguel and A P Zwane (2011), “Spring cleaning: Rural water impacts, valuation, and property rights institutions”, The Quarterly Journal of Economics 126(1): 145–205.
Kremer, M, S Luby, R Maertens, B Tan and W Wiecek (2022), “Water Treatment and Child Mortality: A Meta-analysis and Cost-effectiveness Analysis”, University of Chicago, Becker Friedman Institute for Economics Working Paper 2022-26.
Kwong, L H, A Ercumen, A J Pickering, J E Arsenault, M Islam, S M Parvez, L Unicomb, M Rahman, JDavis, and S P Luby (2020), “Ingestion of fecal Bacteria along multiple pathways by young children in rural Bangladesh participating in a Cluster-Randomized trial of water, sanitation, and hygiene interventions (WASH benefits)”, Environmental science & technology, 54 (21): 13828–13838.
Larsen, B (2016), Benefits and Costs of Drinking Water, Sanitation and Hygiene Interventions, Copenhagen Consensus Center.
Liaw, J, G Marshall, Y Yuan, C Ferreccio, C Steinmaus and A H Smith (2008), “Increased childhood liver cancer mortality and arsenic in drinking water in northern Chile”, Cancer Epidemiology and Prevention Biomarkers 17(8): 1982–1987.
Lokuge, K M, W Smith, B Caldwell, K Dear and A H Milton (2004), “The effect of arsenic mitigation interventions on disease burden in Bangladesh”, Environmental Health Perspectives 112(11): 1172–1177.
Pitt, M M, M R Rosenzweig and M N Hassan (2021), “Identifying the costs of a public health success: Arsenic well water contamination and productivity in Bangladesh”, The Review of Economic Studies 88(5): 2479–2526.
Prüss, A, D Kay, L Fewtrell and J Bartram (2002), “Estimating the burden of disease from water, sanitation, and hygiene at a global level”, Environmental health perspectives 110(5): 537.
Smedley, P L and D Kinniburgh (2001), “Source and behaviour of arsenic in natural waters”, United Nations Synthesis Report on Arsenic in Drinking Water, 1-61.
Stenberg, K, R Watts, M Y Bertram, K Engesveen, B Maliqi, L Say and R Hutubessy (2021), “Cost-effectiveness of interventions to improve maternal, newborn and child health outcomes: a WHO-CHOICE analysis for Eastern sub-Saharan Africa and South-East Asia,” International journal of health policy and management, 10 (Special Issue on WHO-CHOICE Update): 706–723.
Tofail, F, M Vahter, J D Hamadani, B Nermell, S N Huda, M Yunus, M Rahman and S M Grantham-McGregor (2009), “Effect of arsenic exposure during pregnancy on infant development at 7 months in rural Matlab, Bangladesh”, Environmental Health Perspectives 117(2): 288.
Troeger, C, B F Blacker, I A Khalil, P C Rao, S Cao, S R M Zimsen, S B Albertson, J D Stanaway, A Deshpande, Z Abebe and N Alvis-Guzman (2016), “Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the Global Burden of Disease Study 2016”, The Lancet Infectious Diseases 18(11): 1211–1228.
Vahter, M (2008), “Health effects of early life exposure to arsenic”, Basic & clinical pharmacology & toxicology 102(2): 204–211.
Wolf, J, S Hubbard, M Brauer, A Ambelu, B F Arnold, R Bain, V Bauza, J Brown, B A Caruso, T Clasen and J M Colford Jr (2022), “Effectiveness of interventions to improve drinking water, sanitation, and handwashing with soap on risk of diarrhoeal disease in children in low-income and middle-income settings: a systematic review and meta-analysis”, The Lancet 400(10345): 48–59.




